Abstract
Background: Acute myeloid leukemia (AML) is a heterogeneous clonal disease of myeloid progenitor cells resulting from alterations in cell differentiation, proliferation, and renewal. Treatment for young patients and those with favorable-to-intermediate risk remains a combination of cytarabine and anthracycline, while the optimal regimen for the elderly has yet to be established. First-line and salvage combination hypomethylating agents azacitidine or decitabine with BCL-2 inhibitor venetoclax (HMA+Ven) has shown promise for these patients and are becoming standard therapy. We present a cohort from our institution treated with HMA+Ven vs traditional therapy. We hypothesize HMA+Ven leads to improved overall survival (OS) and complete remission with or without count recovery (CR/CRi) compared to traditional therapy in the elderly and those with unfavorable risk as defined by the European LeukemiaNet (ELN-2017) risk stratification.
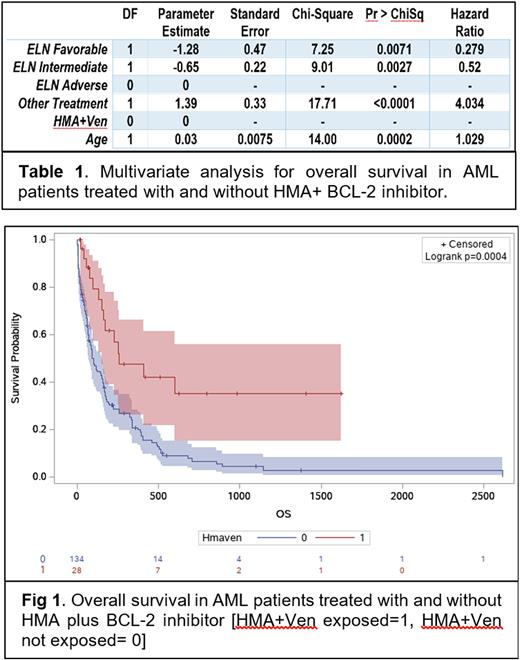
Methods: 232 AML patients from Baylor St. Lukes Medical Center, and Michael E DeBakey VA Medical Center from 8/26/1997 to 7/31/2021 were reviewed. These patients were stratified by HMA+Ven vs. other standard treatment. Differential survival among groups was measured by Kaplan-Meier method. The independent effect of HMA+Ven against multiple intervening variables was evaluated by Cox proportional regression analysis. Chi-square and t-test detected potential intervening variables with impact on outcome. SAS software was used for analysis.
Results: Those treated with HMA+Ven comprised 28 out of 227 patients (12.3%). Average age of patients was 65 (26-80) in the HMA+Ven group and 61.3 (20-93) in the other treatment group (p=0.05). Age, ELN-2017 risk stratification, and HMA+Ven treatment were predictors for survival (Table 1). OS in our cohort favors HMA+Ven vs other treatment (Fig. 1, 348 days vs 261 days, p=0.0004). Overall survival in the elderly population of interest favors HMA+Ven (270 days vs 135 days, p<0.0001). CR/CRi was superior for HMA+Ven in those age >60 (55% vs 24.7%, p=0.006) as well as those age >70 (55% vs 15.2% p=0.007). OS for those with adverse ELN-2017 stratification favors HMA+Ven (352 days vs 164 days, p=.002). Interestingly, overall survival trends for those with active smoking history favors HMA+Ven (p<0.0001). Lastly we found CR/CRi favors HMA+Ven for those with RUNX1 gene mutation (75% vs 25%, p=0.01).
Conclusion: HMA+Ven demonstrated superior response in our elderly patients and those with unfavorable risk through OS as well as CR/CRi, compared to those treated with traditional therapy. This held true across all ELN-2017 risk categories when examined by cox regression models (Table 1) and was most notable in the adverse risk subgroup. The mechanism by which smoking may enhance HMA+Ven survival is uncharacterized and warrants investigation.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal